(The Tennessean, December 1, 2013)
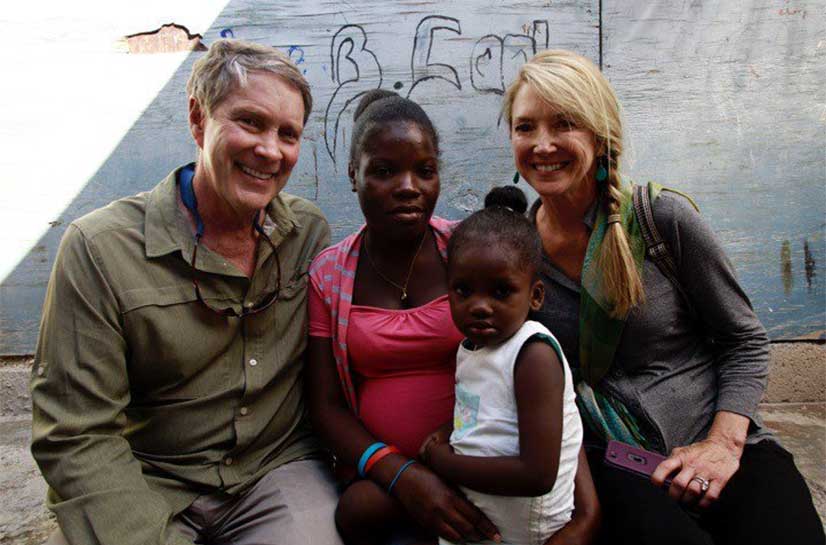
By Sen. Bill Frist, M.D. and Manoj Jain M.D.
Authors’ note: This is the final of six parts. We are honored and extremely grateful that so many shared their family stories with us. We have preserved the stories but have changed individuals’ names.
Over the past three months, as we have journeyed through the difficult topic of “end-of-life care,” we’ve had the privilege of hearing from many Tennesseans. You have shared stories of tender passings, tales of deep struggle, and accounts of sheer confusion and angst at the end of life of a loved one. The personal stories you’ve entrusted to us have renewed our passion and commitment to enable conversations in families, with doctors and in the community that will ensure loving and peaceful experiences at the end of life.
Milly described how this summer her husband suffered a massive stroke, which left him unable to feed himself and, even worse, unable to swallow food without aspirating. Milly and her husband had prepared for such a day because they had endured the painful death of her stepfather the previous summer: an experience in which he was left mute and paralyzed for months in the nursing home.
Include family in plan
Initially, Milly said, her children were alarmed and angered at the thought of forgoing more aggressive treatment in the hospital. While Milly and her husband had signed advanced directives together, they hadn’t shared their plans with the children. Thankfully, when they saw their father’s signature on the advance directive papers their anxiety was eased and they graciously accepted his wishes. Milly describes her husband’s last two weeks at home with hospice as “tough” but infinitely better than being in the hospital or the nursing home.
As with many families, it took a painful experience for Milly and her husband to realize the importance of planning for end of life. We encourage everyone to take the first step now, and not wait for a tragic experience to underscore the need for end-of-life preparation.
Once you’ve made your decisions, share your wishes with your loved ones. Knowing that the choice is yours relieves family of the burden of making difficult decisions.
Joe shared the medical journey of his wife, who was diagnosed with lung cancer and was told she had less than a year to live. She began chemotherapy and for four years enjoyed a good quality of life, able to care for herself and spend precious time with her family. When her tumor spread into her spinal cord, Joe’s wife wanted to continue chemotherapy and simultaneously begin hospice, yet hospice declined. Forced to choose, she ultimately returned home with hospice support and died surrounded by family.
Strings attached
Joe and his family experienced a sad reality in much of end-of-life care: Services are available, but they have strings attached. Hospice is a service offered to Medicare patients at no cost; yet, for patients to be eligible for hospice their life expectancy must be less than six months and they must no longer be taking any active treatments such as chemotherapy.
There is need for a sea change in end-of-life care, and models of palliative care are gaining ground in Tennessee. For example, Aspire Health aims to build a patient-centered comprehensive service that doesn’t demand a choice.
A final story: Grace’s parents’ health declined together over several months. While recovering from a heart attack, her father was diagnosed with rapidly progressing Lewy body dementia. Hospital social workers suggested a nursing home with physical therapy, but after family discussion and much prayer, Grace’s family decided to make the transition to hospice. Grace’s father died in his home surrounded by family.
‘See you soon’
Grace’s mother’s last words to her husband of almost 70 years were “I will see you soon.” She became ill the day of her husband’s funeral, was diagnosed with pneumonia and congestive heart failure, and died six weeks later.
For Grace, the tandem death of her parents seemed “surreal,” but the coordinated care from the primary care team, the hospice team and the home caregivers made it possible to endure those months and glean the best from them.
The experience was also made easier by her father’s meticulous preparations. He had carefully planned for the end of his life, even including a note reminding his family to “call the church sexton (during the funeral) so he’ll open the church so people can go to the bathroom.”
In sharing their stories, Milly, Joe and Grace have given all of us the impetus to learn from their experiences. Health care is complex. We are working within the medical community to increase the options for end-of-life care, but it is up to us all as individuals to initiate conversations about end-of-life wishes with our families.
If you’re still unsure where to begin, Alive Hospice, in Nashville, has launched The Gift Initiative this holiday season, encouraging all of us to give ourselves and our loved ones the ultimate gift of peace and preparation. Resources and free materials are available atwww.thegiftinitiative.org.
For many, the Isaac Asimov quote holds true: “Life is pleasant. Death is peaceful. It is the transition that is troublesome.” But we believe that with thoughtful preparation, peace of mind is available to us all at the time of transition.
Bill Frist is a heart transplant surgeon and former U.S. Senate majority leader. Manoj Jain is a Tennessee doctor who writes for The Washington Post.
Originally posted at: http://www.tennessean.com/apps/pbcs.dll/article?AID=2013312010072