UPDATED: If you missed the event, the entire webinar broken down by speaker is archived online.
On September 10, 1 pm EDT, I and some friends will be speaking at a live, free webinar sponsored by the National Institute for Health Care Management (NIHCM) on palliative care. We certainly need it, but how will the system pay for it? I’ve outlined some of my thoughts below, but we need your voice too! Please join me!
http://www.nihcm.org/improving-access-to-integrated-palliative-care
Palliative care is one of the fastest growing specialties in American medicine today. This growth is driven not only by our aging population but also by the cultural and financial shift in medicine from fee-for-service to value-based care. However, when we talk about value-based care in the palliative care setting what we really have is a chicken-and-egg problem.
Value-based care is traditionally thought of as pay for outcomes. A hospital reduces hospital re-admissions, or a primary care physician achieves blood pressure goals on 80% of his patients and their reimbursement is higher. However, the important question is, How do you even achieve those goals in the first place? And in the palliative care setting—chronically ill patients who are not going to get “better”—What is an improved outcome?
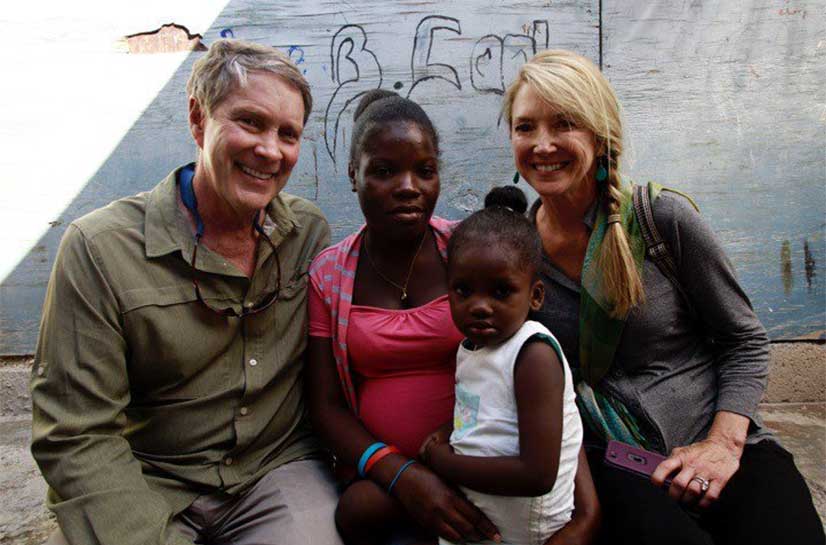
The answer to the first question is a “medical team” model. Keeping patients well, especially the chronically ill, is all about care coordination. In the primary care setting, this means a team may have a physician, a nurse practitioner, a social worker, a registered nurse, a dietician, a psychologist and others all working together to meet the needs of a patient. A patient is not a single illness. Each patient is a person with a family and possibly a job living in a community and dealing with many life stressors of which their illness is only one. You have to address the whole patient with all of their non-medical issues to reach success on their health outcomes.
In a palliative care setting, taking a medical team approach is even more imperative. The goal in palliative care is improved quality of life, which means better symptom management, reduced episodes of acute illness and overall better patient well-being. For chronically ill patients, coordinated care is the only way to achieve this.
If value-based care in the palliative setting means coordinated care, and the outcomes achieved can be cost saving, why isn’t everyone moving to this model? The reason is always the same: current reimbursement models do not support it. We bill for procedures, not outcomes, and even the shift to paying for outcomes is physician-centered. Chaplains and social workers are imperative, but they do not generate revenue under the current model.
We want the outcomes palliative care can offer. We want the cost-savings palliative care can generate. But to do that the payment model has to change, which requires proving to payers that the a medical team approach works, and finding people brave enough to venture into the palliative space when payment is not guaranteed.
The good news is healthcare systems and providers are changing. In Oregon and Colorado Medicaid reimburses for end of life discussions. Palliative care companies and programs within hospitals are springing up around the country. But the system is in transition and we need a more cohesive solution.