(The Week, August 29, 2012)
Lawmakers in D.C. may truly be committed to improving America’s health-care system. But according to actual physicians, our leaders are going about it all wrong
Want real health reform that is in the interest of you and your family? Don’t make the same mistake that Washington did. In formulating ObamaCare, the politicians listened to lobbyists, policy wonks, academics, health theorists, regulators, and occasionally to each other. But they failed to listen to the people who actually care for patients: Doctors. Granted, the lobbyists for physician groups were at the table, but not the doctor him or herself. Ironic, isn’t it? Especially when it’s the doctor who has the daily responsibility of directly caring for the patient.
Go ahead, ask your physician at your next visit what she or he thinks of current Washington-directed reform and its impact on the doctor-patient relationship. What you hear will likely surprise you, because it will likely be markedly different from what you hear from Washington. The policy theorists are simply too far removed from the reality of front-line patient care. Health reform, whether via the implementation of ObamaCare or the GOP’s “repeal and replace” plan, should no longer ignore the input and counsel of experienced, front-line, practicing doctors.
Here is a sampling of what my own internist, who has taken care of thousands of patients over the past 20 years, shared with me:
Frist: We hear the electronic health record (EHR) will solve much of what ails our health sector.
Doctor:
The EHR is not the savior of the medical system. In fact, it is effectively destroying the relational aspect of the art of medicine. Instead of talking with a patient and hearing her “story,” we are being relegated to looking at a computer screen and pointing/clicking during the visit. I know there are long-term benefits to an EHR, but most internists who value the art of medicine will tell you it is killing the “story.” And it is expensive. Physicians with EHRs see 15 to 30 percent fewer patients (and work later into the night). And yet with ObamaCare, we will be asked to take care of an additional 30 million patients.
We are told that increased government regulation and monitoring will reduce waste.
Unnecessary regulations and increased paperwork are drowning us and reducing quality of care. We have allowed just “one more thing” to be added over and over again. The camel’s back is now breaking. I have never seen physicians as depressed and stressed in my 20 years of practice. At each visit, I am required to tell the government whether the patient I am seeing had a flu shot last winter! Please help me understand how that improves care. I know the many quality metrics (i.e.: check this box) mean well, but they are having the opposite effect. They are diminishing quality because they (the boxes) become the focus of each visit, rather than the human interaction.
But increased documentation in charts and billing surely improves value to the patient?
Hardly. We are now working with 17,000 diagnosis/billing codes — absolutely ridiculous. There are nine codes for abdominal pain (right upper, left upper, right lower, left lower — you get the idea). And the government has recently increased the number of codes from 17,000 to 155,000. The bottom line — 300 codes would probably cover everything. It could be printed in a four-page leaflet, not three large volumes. It is unnecessarily complicated and it does absolutely nothing to improve patient care.
Doesn’t more careful documentation with the required codes help eliminate fraud?
That’s ridiculous. It is just the opposite. The actual diagnosis/billing codes have nothing to do with fraud. The EHR creates the appearance of a perfectly prepared note. In truth, it simply makes it easier to copy and paste from note to note. The note is filled with unnecessary information, making the truly pertinent information hard to find (and therefore negatively impacts patient care). The nice-looking, “electronic documentation” in the EHR opens the door for the unethical doctor to game the system and get away with it. It just makes it easier for them to upcode and not get caught. Fraud is skyrocketing while the EHR provides the cover.
But Washington tells us that “evidenced-based medicine” is the surest way to better outcomes.
Quality care comes from a careful, professional analysis of a clinical situation that leads to a correct diagnosis and treatment for the particular patient at hand. Quality care will never be found by mindlessly marking boxes or following algorithms that are at the heart of what is being called “quality measures and evidence-based medicine.”
What stands between you and caring for the patient?
The paperwork is overwhelming — nursing home admission forms, medical device forms, diabetic supply forms, home health forms, insurance records requests for “additional information.” Everyone has their form that must be completed. All forms roll downhill and the internist is the final resting place. Regulations requiring more needless paperwork mean less time for patients.
The law in Washington is that your reimbursement is to be cut every year. But you seem to be working harder than ever.
Reimbursement for our services continues to decline, because overhead costs rise. I am very blessed. I am paid well. But I have not seen a raise in 13 years. While CEOs, managers, administrators, benefit managers, and insurance executives see regular raises and bonuses. Physicians in our clinic feel fortunate that our pay has not declined. Yet our workload is so much heavier than it once was. Not because of patient volume, but because of the higher expectations of patients, the higher complexity of medical care, and the excess “stuff” that we are being required to do.
I’m told the primary care shortage of 40,000 doctors over the next 10 years can be met by non-physicians.
The suggestion that non-physician practitioners can fill the primary care needs of the American people is simply false. Their training, knowledge base, and ability to form a complete differential diagnosis is limited. The press often proclaims that nurse practitioners can replace doctors. There is a role for the NP and we need to support that role. But to suggest that someone with two years of training can provide equivalent care to that of a physician who, after college, has spent four years in medical school, three to four years in residency (working days and nights), and who, each day, makes hundreds of decisions for which he or she is ultimately responsible is not only wrong, it disrespects the training and ability of the physician. Remember, quality care is not measured by patient satisfaction surveys, but instead, by the ability to properly diagnose and treat a patient.
So… we’re not moving in the right direction with health reform?
At the age of 49, I feel that the practice of the art of medicine is becoming impossible, even for those of us who live for the chance to care for others. Our goal should never be to cure disease. Instead, our goal should be to heal people. The direction of our present system is negatively impacting the ability of good doctors to try and heal people. We must remove the growing distractions and be allowed to spend time with each unique patient and their “story.” We need to ask of each regulation or mandate that “seems” to sound so good: How will it impact the doctor-patient relationship? It is now, and will always, be within this relationship that healing occurs and true quality care is found.
—
Those are the words of one, but they are the sentiment of many. Ask and see.
And what is interesting is that this sort of conversation from the front-line would never make it all the way up to my office when I was majority leader of the U.S. Senate. The existing, overly restrictive filters of Washington lobbyists and bureaucracy simply don’t allow such real-life information to flow all the way up to the legislator.
So for the next round of reform, let’s make sure we don’t ignore the insights of real-life doctors. Let’s make sure this time around they are at the table.
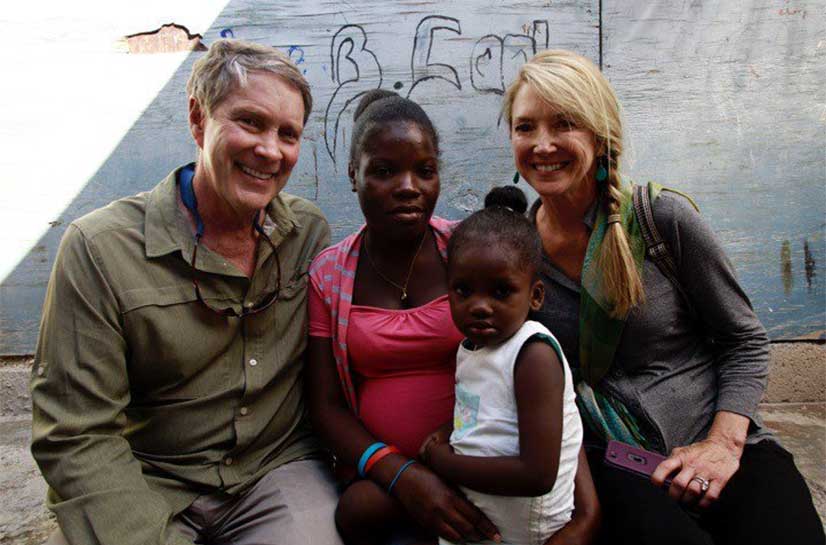
Dr. William H. Frist is a nationally acclaimed heart transplant surgeon, former U.S. Senate Majority Leader, the chairman of Hope Through Healing Hands and Tennessee SCORE, professor of surgery, and author of six books. Learn more about his work at BillFrist.com.
This article was originally featured in The Week http://theweek.com/article/index/232510/what-my-doctor-thinks-of-obamacare