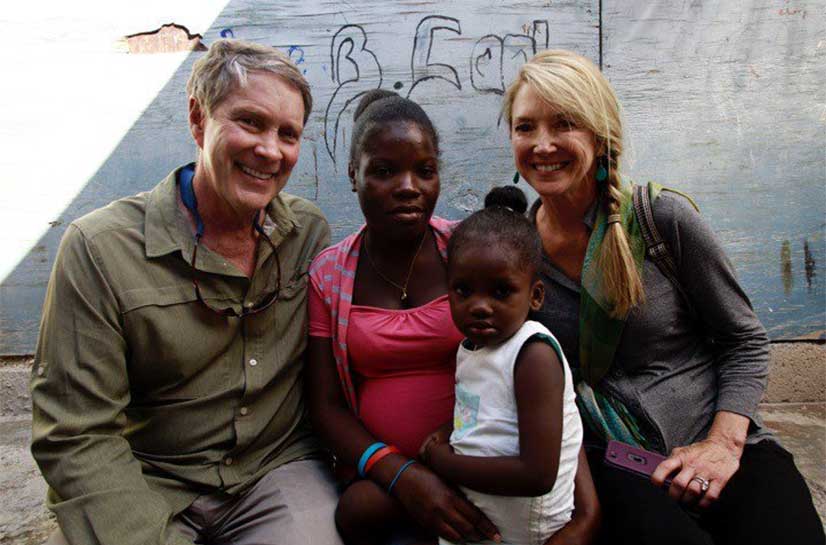
By Bill Frist and Dr. Manoj Jain
We have done it. We have decreased the increase in the cost of healthcare. Let us explain. For three decades (1980–2009), the cost of healthcare has been increasing each year at an average rate of 7.4%—double the rate of inflation. However, over the past three years, the increase in healthcare expenditures has remained at a low 3.1%.
Is this decline the desperately needed bend in the healthcare cost curve or just the impact of the depressed economy?
Four leading studies point us in different directions. Last month’s Kaiser Family Foundation study deduced that 77% of the decline was attributable to the economic downturn and is likely temporary. A report by the Robert Wood Johnson Foundation echoed these conclusions.
In contrast, two articles in the May issue of Health Affairs point to structural changes such as “less rapid development of imaging technology and new pharmaceuticals, increased patient cost sharing and greater provider efficiency” as major causes of the decline, suggesting that only 40% to 55% of the decline was because of the economic downturn.
The final answer is probably somewhere in between, with about half of the decrease realized by encouraging changes in the way healthcare is delivered and the other half due simply to the downturn in our economy. Regardless, it is important to recognize—and celebrate—that the cost curve has bent without collapsing our healthcare system or being prompted by draconian measures in rationing of healthcare. Moreover, the decline has not led to deterioration in our quality measures. In fact, they have improved.
Now, the $2.7 trillion question is, “How can we sustain this slower growth over the next decades?”
Undeniably, during the past several years, the singular focus of conversation among policy makers has shifted from simply more care and better quality of care to better value in healthcare, where value is defined as quality over cost. The onset of value-based purchasing by Medicare and higher copays and deductibles for patients in employer-based plans has helped in disseminating this message to doctors and patients.
Yet if history is any indicator, the cost of healthcare will rise once again as our economy strengthens. So, last month the Bipartisan Policy Center made 50 bold recommendations on how to sustain the lower growth of healthcare costs. These recommendations are unique because they focus on improving the entire system of care over a prolonged period of time and break through the partisan rhetoric surrounding healthcare reform.
We want to highlight a few of the recommendations that will impact providers—hospitals and doctors. The BPC encourages advancing accountable care organizations to a 2.0 version where the entire spectrum of patients’ needs would be covered for a fixed payment, and in doing so replace the irrational and outdated sustainable growth-rate formula for physician reimbursement.
Also, the BPC policy paper suggests changing our present voluntary bundle payments program to the standard method of payments for certain DRGs. The impact of such a change in the payment system can be profound. When in the 1980’s Medicare changed payments to hospitals by DRG, length of stay and hospital payments declined.
If such measures are not successful in restricting the cost of healthcare, then a fallback spending limit or a “cap” would take effect based on annual per beneficiary spending growth to a target of GDP.
To sustain these reductions in cost, the availability of current cost data and transparency of such data are essential. At present when patients get their bills, they do not know the difference between healthcare charges, expenditures and costs. To borrow an analogy from car sales: the sticker price, the new owner’s price and the dealer’s invoice price, respectively.
As for providers, physicians are often unaware whether an antibiotic costs $150 or $15 when writing the prescription or a doctor’s order in the hospital chart.
These costs have real impact for Americans. One RAND Corp. study found that if healthcare costs had risen at the slower rate equal to the Consumer Price Index, an average American family would have had an additional $5,400 more to spend each year on education, entertainment, food and clothing over the past decade. But instead, the average family has spent that money on healthcare. With our healthcare system at this crucial crossroads, we need to take this opportunity and stop the collateral damage.
A slower growth of healthcare cost would mean less burden on the individual family, freeing that family to invest in and live a higher quality of life. And for communities it would free billions of dollars for education, businesses, job creation and future innovation.
The good news is that it can be done. And the blueprint for eliminating waste, lowering the cost and maximizing the value is actively being considered by voices that rise above partisan bickering.
Manoj Jain is an infectious disease specialist in Memphis, Tenn.
Bill Frist is a heart transplant surgeon and former U.S. Senate majority leader.
This article was originally published in Modern Healthcare.