(The Week, Sept 11, 2012)
It’s a fraught question, but unless we move beyond caricatured “death panels” and deal with grim realities thoughtfully and responsibly, we’re all in trouble.
How do you envision death with dignity? I like to think of being at home in the comforting and supportive environment of family and friends. But the odds are that neither you nor I will leave this world as we might wish — unless policymakers change course.
End-of-life care is perhaps one of the most complex, emotional, and delicate issues in all of health care. Those final weeks and months can be an incredibly challenging and, too frequently, confusing period for us. At a time we hope for peace, tranquility, and dignity, a patient is often pulled in opposing directions by doctors, intensive care unit treatment options, family and friends, and by the demands of one’s own — at times excruciating — pain, and stubborn defiance.
My perspective comes as a surgeon who by the nature of my specialties of heart disease and cancer has walked with hundreds of patients and their families though these final days of life. It is never easy.
Now is the time for a national conversation on how we should allow death to unfold. Why now? Because in this technology-driven age of high expectations, we are losing patient autonomy and dignity in dying — and it is costing each of us a lot. This is a discussion important to us as patients, families, care givers, and policymakers whose responsibility it is to set a framework where autonomy and dignity in both healing and death are maximized.
The discussion must rise above the rhetoric of “death panels” and partisanship; it must be civil, inclusive, and thoughtful. It must include respect for every individual patient’s wishes, consideration of often complicated family dynamics, and the roles of doctors, nurses, and healthcare providers. And yes, in this day and time of miraculous but expensive technology, the conversation must include the recognition that our society cannot afford the skyrocketing cost of inappropriate end-of-life care.
Just last week, a grieving son asked me how it is even possible that the last two months of his 93-year old mother’s life could cost $200,000 in medical bills when his mother, suffering from fatal cancer, wanted no further extraordinary treatment. Surely there is a better way. But what are the solutions?
Cost of healthcare is a challenging issue because solutions often suggest fewer services or “less care.” But increasingly, we learn that is not the case; they can mean more appropriate care. Cost discussions become especially sensitive when it centers on care and treatment at the end of life. But in reality cost is an issue —– especially when tied to futile spending which detracts from the patient’s wishes and the dignity of death and dying.
Part of the cost problem is the low barrier to expensive, but truly miraculous and potentially life-saving, technology. I have lived it. My medical specialty included lung transplants, artificial hearts, and mechanical extracorporeal circulation. Such advances have tremendously improved American medicine. Over the last 50 years, average lifespan has increased two months every year! We live almost 10 years longer today than we did in 1960. We routinely transplant hearts into patients who would otherwise die within a month, and they live an additional 20 years. Fathers doomed to death live to watch their daughters marry and have children. But technology comes with a hefty cost, if misused.
Here are the facts: 30 percent of Medicare dollars are spent in the last months of life. That amounts to more than $150 billion annually. On top of that, a quarter of Medicare recipients spend more than the total value of all their assets on out-of-pocket health care expenses during the last five years of their lives. Every day in an intensive care unit can cost $10,000. Nearly 1 in 5 Americans spend their last days in an ICU.
Technology and intensive care treatment have limitations when misapplied. People spend fortunes on the last months of life. The high expectations and demands of grieving family members fuel this process. And because someone else is always paying, it is inevitable that unnecessary tests and procedures and high-intensity services creep into the equation. The system is set up and incentivized to bend to the whim of an unusual family member’s demand to “keep mom alive at all costs,” even if she is 93 and hopelessly ill.
So how do we fix all this? We begin a national, high-profile, civil dialogue, which should begin in the living rooms of patients and their families and extend to nurses’ and doctors’ offices, hospitals, religious institutions, and policy chambers. “How do I want to die?” That’s the framing question. It’s a tough place to start, but grounds the discussion in the reality that unless we act, our final days will be spent very differently than we would like.
Ventilators, mechanical heart assist devices, high-tech intensive care units, and powerful medicines provide the means of postponing the inevitable, usually uncomfortably and at high cost, while stripping away independence and dignity from those final days. Do we want to die at home or strapped to machines in a hospital bed? How much quality of life, how much loss of normal function, are we prepared to live with? Does my husband or daughter know my wishes?
Here are three proposals we should include in the conversation.
1.
Each of us must act to assume responsibility for expressing our preferences and intentions up front. Act today. Begin with establishing a written “advanced directive” to make your intentions clear. One type of advanced directive is a living will, which applies if you become incapacitated and lack competency to decide medical questions for yourself. Another important advance directive is the “durable healthcare power of attorney,” which designates a person to make medical decisions for you if you have not signed a living will or other directive.
Four out of five of us have not done this. These important legal documents provide an essential roadmap for your preferences and relieve your family and your doctors from having to guess what you would really have wanted and help resolves conflicts among family members. Share your values and intentions directly with your doctor, your family, and leader in your life.
2.
Medical education for our caregivers must be reformed to more specially address end-of-life issues. Many doctors and nurses are inadequately trained to lead families though these challenging times. How do you determine when further care is futile and then compassionately communicate the moment when technology adds no value, and in fact detracts from the dignity of life? How do you handle the well-intended-but-unreasonable family member who demands “more care” when the science says it’s futile? A physician, nurse, or hospital will worry about a lawsuit if the armamentarium of high technology is not exhausted even though evidence-based medicine says it is a waste of resources.
My physician dad and earlier generations of doctors were not confronted with a health service environment so complex and replete with alternatives as ours. In their day, medical science was inexpensive and limited in scope. They had less technology at their fingertips. Today’s physician requires more training in end-of-life communication and evidence-based decision-making.
3.
Expand both palliative and hospice care. Hospice provides compassionate and appropriately specialized care for those who will soon die. The setting is typically at home. Palliative care is a new specialty grounded on a multifaceted team-approach to comprehensively manage severe, often long-lasting chronic disease and persistent pain and suffering. Both center on autonomy and dignity and appropriate medical and social care for a particular patient’s medical condition. Both are based on science and evidence-based medicine. Both have been shown to improve patient satisfaction, reduce pain and discomfort, and improve quality of life.
Expansion will require rethinking reimbursement mechanisms to allow scalability. How do these two models fit within more integrated health systems? How should caregivers be compensated for providing more appropriate care but not more procedures and more technology?
Isaac Asimov wrote, “Life is pleasant. Death is peaceful. It is the transition that is troublesome.” It is time to focus on the transition. No one has the answers yet. But we can find them together. The way to begin is to initiate a rational national dialogue, as uncomfortable as the conversation may seem to be.
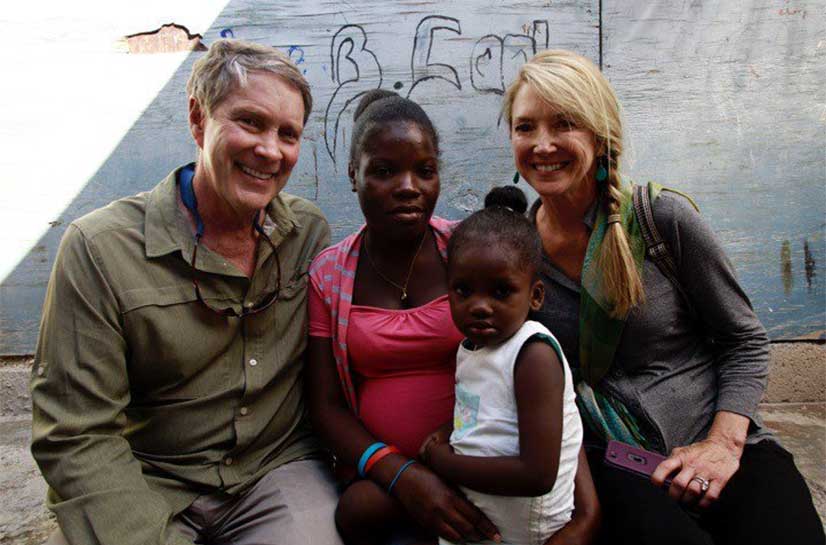
Dr. William H. Frist is a nationally acclaimed heart transplant surgeon, former U.S. Senate Majority Leader, the chairman of Hope Through Healing Hands and Tennessee SCORE, professor of surgery, and author of six books. Learn more about his work at BillFrist.com.
This article was originally featured in The Week http://theweek.com/article/index/233111/how-do-you-want-to-die