Nov. 21 (Bloomberg) — Bloomberg View columnist Lanhee Chen is joined by former U.S. Senate majority leader William Frist, Mayo Clinic CEO John Noseworthy, Boston Consulting Group partner Michael Ringel, John Hopkins Medicine CEO Paul Rothman, Thompson Holdings CEO Tommy Thompson, and Walgreen CEO Gregory Wasson to discuss the state of healthcare in the United States. They speak at Bloomberg’s The Year Ahead: 2014 conference at the Art Institute of Chicago.
Archives
Elderly need options for palliative care
(The Tennessean, October, 20, 2013)
By Sen. Bill Frist, M.D. and Manoj Jain, M.D.
A patient — we will call her Matilda — has thin, silvery hair, deep-set eyes and is in her mid-80s. She worked as a factory worker until she was widowed and now lives alone a few miles away from two working daughters.
Matilda’s swollen body reveals some of the health challenges she faces. She has congestive heart failure and recurrent blood clots, both of which cause swelling in her legs and led to a hospitalization a few months ago for a skin infection. She improved and went home and with help still managed her own care: orchestrating a dozen medications daily, including a blood thinner, her cooking and frequent doctor appointments.
A few weeks ago, she contracted pneumonia, probably caused by aspiration — food going down her windpipe rather than her esophagus — probably during a minor stroke. She was admitted to the intensive-care unit but just avoided intubation and being connected to a ventilator.
Now, Matilda is better. She does not want aggressive treatment such as a ventilator or life resuscitation. She does not want to be in a nursing home. She does not have a terminal illness. As the time for her discharge from the hospital nears, the question for her daughters, her doctors, the social workers is: Where should she go? Who will care for her? No model of care seems to work well.
Our present model of health care focuses on either providing life-prolonging aggressive care regardless of quality of life in the hospital and ICU setting, or providing hospice care when patients have a life expectancy of less than six months. For patients who are slowly declining, a nursing home may be their only option for getting the support they need.
Matilda and millions of other elderly Americans do not fit into these molds. They deserve better options than these.
A new option to consider
Palliative care is one such option that seeks to intervene early in the course of chronic illness; to ease the patient from a curative goal to a comfort goal; and to meet medical, social, psychological, spiritual and family needs. Over time, if the illness becomes terminal, the patient is moved to hospice care.
The palliative care model is still relatively new in the U.S. Under this model, Matilda’s primary care physician would work closely with a palliative care physician, nurse practitioner, nurse, social worker and even a chaplain. Together, the palliative care team would manage Matilda’s medicines, answer calls in the middle of the night and work to prevent hospital readmission. The team’s dual focus is on making her comfortable and continuing full medical treatment of her conditions.
A network of resources treats the progression of the illness while trying to avoid emergencies. Instead of jumping from one crisis to the next, leaving Matilda disoriented and fearful, palliative care provides her with continuity of care and support.
So why do we not see more health providers, hospitals and doctors offering palliative care services?
The major stumbling block is payment methods. The current structure of Medicare and Medicaid is fee-for-service reimbursement instead of focusing on the whole patient and providing care such as frequent home visits and 24/7 telephone support. Since most insurance plans take their cue from these federal programs, they don’t support palliative care, either.
There is one new piece of legislation that would begin to address this need: The Care Planning Act, S. 1439, sponsored by U.S. Sens. John Isakson, R-Ga., and Mark Warner, D-Va., and introduced in August. It would amend the Social Security Act, which encompasses Medicaid and Medicare, and it would provide specific compensation to physicians for one-on-one, end-of-life planning discussions with their patients. While this would certainly help encourage physicians to take the time to have these conversations, the services planned and needed still require support.
The bill supports pilot palliative care programs, which would deliver coordinated palliative care including an interdisciplinary team, 24/7 telephone support and home visits. Once a successful pilot emerged, then a systemwide solution could be implemented.
While The Care Planning Act is a step in the right direction, it still comes with a price tag. Yet, the financial benefits of a palliative care model with fewer hospital admission and ER visits would outweigh the costs. Given that these savings come with longer life expectancy and a better quality of life at the end of life, palliative care programs are not just a benefit, but also a necessary addition to our medical model.
Over the past several weeks, we’ve encouraged everyone to discuss end-of-life issues with their families and physicians. Initiating these conversations ensures that your family is aware of your wishes, and that hard decisions can be made with peace of mind.
End-of-life care is not only an issue facing us as individuals, though: The health care system also has reached a critical mass. High costs and low patient value are not sustainable. It’s time for a different model of care.
Bill Frist is a heart transplant surgeon and former U.S. Senate majority leader. Manoj Jain is a Tennessee doctor who writes for The Washington Post.
This article was originally featured in The Tennessean on October 20, 2013 http://www.tennessean.com/apps/pbcs.dll/article?AID=2013310200075
We often avoid important conversation
(The Tennessean, October 6, 2013)
By Sen. Bill Frist, M.D. and Manoj Jain, M.D.
When a patient’s lymph node biopsy came back as a rare form of lymphoma, he did not have long to live. In the six months before he died, he did not settle his family affairs or financial accounts. His doctors should have initiated a frank conversation to best equip him to plan for his remaining time.
End-of-life conversations between patients and their doctors are not happening often enough. A 2009 Archives of Internal Medicine study of patients with terminal metastatic lung cancer (the majority of whom lived only two months after they were interviewed) found that just slightly more than half of their health care providers had discussed hospice care with them.
Every patient will face the end of life. So why don’t all doctors discuss options for end-of-life care with their patients?
In this patient’s case, I know why his physicians did not push harder for such a conversation. They were hesitant to give him a timeline for the course of his illness. They were not ready for the final prognosis. They planned to talk about it later.
I (Dr. Jain) know this was the case because I was one of his physicians. And I wish I had pushed early for an end-of-life conversation.
Unready for prognosis
Doctors are conflicted because — in most cases — forecasting a timeline is hard to do, even among the most experienced clinicians. For a patient awaiting a heart transplant, the outcome without a donor organ is very clear. But several studies have suggested that when dealing with many terminal illnesses, especially cancer, doctors are usually incorrect in their prognosis, nearly always tending to believe that their patients will live longer than they actually do.
Harvard Medical School professor Jerome Groopman, a leading cancer and AIDS researcher, says that when he is really pressed, he will provide a likely timeline. But he adds, “You want to partner with (your patients), not be the presiding judge handing down a death sentence.”
End-of-life conversations between patients, families and the doctor require quiet time, in the clinic or the hospital, time found amid good days and bad days of chemotherapy, congestive heart failure treatment or progressive dementia. The right day for the conversation often never seems to come.
Many doctors, especially those trained more than a decade or two ago, have had no guidance on when and how to talk with patients about the end of life. We were trained only to prolong life, not help in its end. Our focus has been on quantity of life, not quality of life.
Patients also avoid the topic. In a 2005 AARP survey of Massachusetts residents over age 50, nearly 90 percent said they wanted honest answers from doctors, but fewer than 20 percent had discussed their end-of-life wishes with their physicians.
How do we overcome this twofold barrier? How can we encourage doctors to initiate the conversation, and patients and their families to ask for the conversation?
Trust is the fundamental basis of the doctor-patient relationship. The patient must trust the doctor and the plan of treatment — or lack of treatment.
Time to reflect
Conversations this important require time to reflect on the trajectory of treatment and the patient’s quality of life. Such conversations are best held in a noncrisis situation, before an ICU admission or emergency surgery.
The doctor can begin by saying something like: “I know this has been hard, but I want to take the time and discuss what your wishes are if the heart failure does not respond to stronger medications.”
Patients can also initiate the conversation with, “I know things are not going well with the treatment and I want to talk about some of my options for end-of-life care that would not involve more aggressive medicines or surgery.”
The Tennessee Department of Health website (health.state.tn.us/advancedirectives) and most hospitals provide a form for physician orders for scope of treatment, also known as the POST form. It is completed by health care professionals and provides a doctor’s order about a patient’s wishes.
For example, POST forms document if you do not wish to receive CPR, antibiotics or medically administered fluids and nutrition.
The POST form records the conversation between doctor and patient, just as an advance care plan (or living will) form records the conversation among families.
Stating your wishes does not mean the end of care. New areas of medical care, including palliative care, are focused on helping patients, families and doctors navigate the end of life in comfort and peace.
As doctors, we always hope to make the best decisions for our patients. In looking back over the care we’ve chosen for our patients, we don’t often question our choice of antibiotic or a surgical technique, but we do wish we had spent more time talking to them about planning for the end of life, before the end of life.
Manoj Jain is a Tennessee doctor who writes for The Washington Post. Bill Frist is a heart transplant surgeon and former U.S. Senate majority leader.
This article was originally featured in The Tennessean http://www.tennessean.com/apps/pbcs.dll/article?AID=2013310060057
It’s Common Sense to Come Together for Our Kids
(The Huffington Post, October 2, 2013)
By Sen. Chris Dodd and Sen. Bill Frist, M.D.
When we served together in the Senate, we found ourselves on different sides of a variety of issues. But when it came to common-sense measures that benefitted our country and our citizens, we pulled together.
We were proud to cosponsor the Organ Donation and Recovery Improvement Act because we knew its reforms would help save thousands of lives in America. Today, we’re pulling together to support another common sense measure — early education for all children in America.
There is little debate that education is key to a child’s future success, or that it is key to our global competitiveness as a nation. But one of the most overlooked ways to improving educational opportunities in America is reaching kids early enough.
Two out five children in America have had no preschool or kindergarten education by age 5. When these children do enter school, many are already behind their peers.
As science has clearly shown in recent years, most brain development is complete well before a child enters kindergarten. Without early learning opportunities, many children are entering school without the tools they need to stay on track and succeed.
Unfortunately, poor children in America are most likely to lose these critical opportunities. As a result, children from low-income families can easily fall 18 months developmentally behind children from middle-class families by the time they’re just 4 years old.
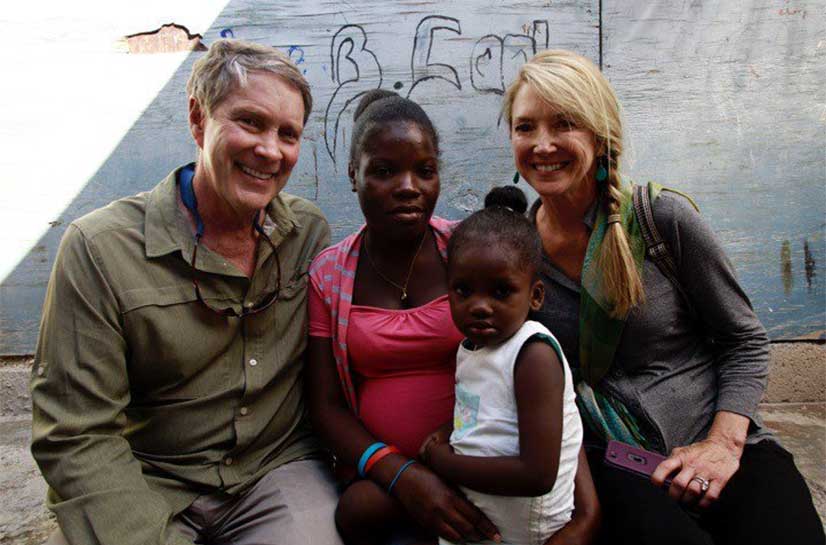
Let us share one anecdote from our friends at Save the Children, to show just what a difference early learning can make. The non-profit organization recently received a letter from the superintendent of an isolated, rural school district in Alpaugh, California.
Poverty, language and cultural barriers, and lack of parental engagement in the education system have long meant that children in the district enter school ill-prepared to succeed, he said.
But this year, he reported, the first group of children who had been through Save the Children’s early learning program entered the first grade. Every one of them is reading at grade level, he said, “something unheard of in past classes.”
This success is particularly significant because research is clear about the importance of reading at grade level by the time a student enters the 3rd grade.
Helping all families have access to children’s books and information on how they can support their child’s development goes a very long way. And giving more children the chance to attend high-quality preschool is the smart thing to do.
One study found that every public dollar spent on preschool returns $7 through increased productivity and savings on government assistance programs and criminal justice costs.
We all have a role to play in helping more children succeed. That can be through volunteering in our own communities, contributing to programs that make a difference, or voicing support for proposals to expand high-quality early education in America.
There is critical work taking place in our country to improve K-12 public education. However, there is more to do to ensure millions of children do not fall behind before they even reach school. Common sense tells us, investing in our children early is the right thing to do.
This blog post is part of a series produced by The Huffington Post and Save the Children, as part of the latter’s drive for universal early education, which is the focus of their gala on October 1 in New York. For more information about Save the Children, click here.
This article was originally featured in The Huffington Post http://www.huffingtonpost.com/chris-dodd/its-common-sense-to-come-_b_4031431.html
It’s never too early to discuss your final wishes
(The Tennessean, September 22, 2013)
By Manoj Jain, M.D. and Sen. Bill Frist, M.D.
A week before my (Dr. Jain) elderly parents came for a long visit, I asked them if they would be willing to have a conversation about end-of-life planning. But it wasn’t until the day before they left that we sat at the dining table with documents I had printed from the Tennessee Health Department website.
Too often among family, such end-of-life conversations do not occur. Studies show that 60 percent of people say they do not want to burden their families with difficult end-of-life decisions. More than 80 percent of people agree that it is important to have end-of-life instructions in writing. Yet less than 25 percent of people have followed through with written directions to ease the burden on their family members.
Why do we not have this crucial conversation? Talking about end of life is certainly uncomfortable. Yet, there may be an even greater fear. Talking about death may be akin to opening Pandora’s box, or being perceived as someone who is encouraging or wishing for our loved one to die.
But by having a conversation about death, we are not inviting or encouraging death for our loved ones, we are profoundly affecting how the end of life will be experienced by everyone involved — both the individual whose wishes are to be respected, and all of the family members who carry their memory forever.
I (Jain) feared that my parents might misunderstand my intentions. As we sat at the dining table, I broke the ice by talking about the death of my grandfather at 93, and how he was clear in his wishes not to go to die in a hospital. My father then told me how he spent the final day and hours with his father, sitting with him. As our conversation went on, I realized that my parents, too, had desired to have an end-of-life conversation.
Whether you are concerned about an elder family member, or preparing to share your own end-of-life wishes, there are resources and tips to make the conversation easier.
Starting the conversation
Approach the topic directly and gently. Start the conversation with plenty of time, on common ground, perhaps by discussing a shared experience. Confirm your desire for a family member’s wishes to be honored, for their dignity to be preserved.
The Tennessee Department of Health provides further guidance for this conversation in its “Five Wishes” resource. More than 18 million “Five Wishes” packets have been distributed.
A structured document called an advance-care plan, or living will, can help guide the conversation. While it is a legal document reflecting our wishes, an attorney is not required to draft it or sign it. In Tennessee, advance-care plans are available online: http://health.state.tn.us/advancedirectives/.
An advance-care plan requires three major decisions. First, an individual must name an agent. A health care agent is a person who will make health care decisions for you. You can make this effective at any time. An agent is usually a trusted friend or relative who you feel will make the best decisions on your behalf.
Next, an individual must determine how he or she defines quality of life in the final days. You decide which conditions are acceptable to you: permanent unconsciousness, such as in a coma; permanent confusion, like end-stage dementia; or dependency for activities of daily living. These are not easy decisions, and over time your opinions may change. Having a frank and thoughtful conversation about your wishes will empower your family if any of those situations arise.
Treatments and Interventions
Finally, individuals must decide which treatments and interventions they would like to take advantage of. At the end of your life, do you wish to receive CPR? Life support? Surgery? Tube feedings? Advance-care plans offer explanations and definitions of each option. If you have questions, your local doctor or nurse can help.
The final product — a two-page document — will be notarized or signed by two witnesses. Then copies should be shared with your physician, your health care agent and close relatives.
Culturally, it is hard for us to talk about and prepare for death, but taking the time to prepare now will be invaluable for you and your family later. Conversations about end of life do not need to be single, marathon affairs. Express your wishes, do your research, discuss again as circumstances change. It is never too early to agree together to a plan, but it could be too late.
Dr. Manoj Jain is a Tennessee doctor who writes for The Washington Post. Dr. Bill Frist is a heart transplant surgeon and former U.S. Senate majority leader.
This article was originally featured in The Tennessean http://www.tennessean.com/apps/pbcs.dll/article?AID=2013309220100
California Cycling
I finished my 75 mile ride from San Francisco to the Red Woods near the Russian River. Now, it is time to enjoy nature and great conversation.
How to Build a Better Health-Care System
(Washington Post, April 17, 2013)
By Tom Daschle, Bill Frist, Pete Domenici, and Alice Rivlin
Tom Daschle, a Democrat and former senator from South Dakota, was Senate majority leader from 2001 to 2003. Bill Frist, a Republican and former senator from Tennessee, was Senate majority leader from 2003 to 2007. Pete Domenici, a Republican and former senator from New Mexico, was chairman or ranking minority member of the Senate Budget Committee from 1981 to 2003. Alice Rivlin is a former director of the Congressional Budget Office. The four co-chair the Bipartisan Policy Center’s Health Care Cost Containment Initiative.
The four of us came together to change the conversation around how to improve health care and constrain cost growth. What we learned is that, until better care is prioritized over more care, our nation will continue to face a problem with health-care costs. The good news is that, through thoughtful policy, health-care practitioners can be encouraged through rewards to focus far more on what is best for their patients and less on the number of tests and procedures they can order. The even better news is that such a health-care vision can not only produce better care but also cost less.
With the Bipartisan Policy Center, we will release a report Thursday with more than 50 recommendations to achieve the critical goal of improving the quality and affordability of care for all Americans while containing high and rising health-care spending. This report is the culmination of nearly a year of work, including stakeholder outreach, thorough research and substantive analytics to quantify the impact of our proposed policies.
Too often we in Washington talk about health care as though it is little more than a line item on a budget table. Those of us who have experienced the best of health care know that is not how care should be delivered or policy crafted in this most personal of issues. Our country can achieve a higher-value health-care system — meaning both higher quality and greater efficiency.
Health-care cost drivers are complex and interwoven, but the most problematic ones we identified are the inefficiencies, misaligned incentives and fragmented care delivery in the current fee-for-service reimbursement system. To address these, we seek to promote coordinated and accountable systems of health-care delivery and payment, building on what has proved successful in the private and public sectors. Organized systems of care emphasize the value of care delivered over the volume of care. These systems are often better able to meet patients’ needs and desires and are able to effectively reimburse providers and practitioners for delivering high-quality care.
In all our proposals, we sought to avoid simple cost-shifting as a means to generate federal budgetary savings, instead promoting transparency and protecting patient choice. We also focused on reforms that will incite transformation across the health-care system, not limited to Medicare. We believe, however, that the power of Medicare can be leveraged to lead the way in transforming U.S. health care.
In brief, our recommendations:
●Preserve the promise of traditional Medicare while adding more choices and protections for beneficiaries, including accountable systems of care and a stronger, more competitive Medicare Advantage program.
●Strengthen and modernize the traditional Medicare benefit, including adding a catastrophic cap, rationalizing cost-sharing and premiums and expanding access to assistance programs for those with low incomes.
●Reform the tax treatment of health insurance to limit the taxfavored treatment of overly expensive insurance products.
●Empower patients by promoting transparency that is meaningful to consumers, families and businesses, and streamline quality reporting.
●Advance the nation’s understanding of potential cost savings from prevention programs, through support for research and innovation on effective strategies to address costly chronic conditions.
●Offer incentives to states to promote policies that will support a more organized, value-driven health-care delivery and payment system, such as supporting medical liability reform and strengthening their primary-care workforce.
All of these policies are designed to improve the quality and value of our nation’s health care. That is where every health-reform effort should start. The savings that we achieved — $560 billion over 10 years in debt and deficit reduction — is the outgrowth of our work, not the goal.
No single set of recommendations can fix the health-care system or the nation’s debt and deficit crisis overnight, but we hope this report can start a constructive, pragmatic dialogue among policymakers and political leaders. By presenting this report to federal, state and private-sector leaders, we hope to promote a collaborative dialogue and a shared understanding of strategies to put our nation’s health system, as well as its economic outlook, on a sounder, healthier and more sustainable path.
This article was originally published in the Washington Post http://www.washingtonpost.com/opinions/how-to-build-a-better-health-care-system/2013/04/17/a44dd478-a6d1-11e2-8302-3c7e0ea97057_story.html
How do you want to die?
(The Week, Sept 11, 2012)
It’s a fraught question, but unless we move beyond caricatured “death panels” and deal with grim realities thoughtfully and responsibly, we’re all in trouble.
How do you envision death with dignity? I like to think of being at home in the comforting and supportive environment of family and friends. But the odds are that neither you nor I will leave this world as we might wish — unless policymakers change course.
End-of-life care is perhaps one of the most complex, emotional, and delicate issues in all of health care. Those final weeks and months can be an incredibly challenging and, too frequently, confusing period for us. At a time we hope for peace, tranquility, and dignity, a patient is often pulled in opposing directions by doctors, intensive care unit treatment options, family and friends, and by the demands of one’s own — at times excruciating — pain, and stubborn defiance.
My perspective comes as a surgeon who by the nature of my specialties of heart disease and cancer has walked with hundreds of patients and their families though these final days of life. It is never easy.
Now is the time for a national conversation on how we should allow death to unfold. Why now? Because in this technology-driven age of high expectations, we are losing patient autonomy and dignity in dying — and it is costing each of us a lot. This is a discussion important to us as patients, families, care givers, and policymakers whose responsibility it is to set a framework where autonomy and dignity in both healing and death are maximized.
The discussion must rise above the rhetoric of “death panels” and partisanship; it must be civil, inclusive, and thoughtful. It must include respect for every individual patient’s wishes, consideration of often complicated family dynamics, and the roles of doctors, nurses, and healthcare providers. And yes, in this day and time of miraculous but expensive technology, the conversation must include the recognition that our society cannot afford the skyrocketing cost of inappropriate end-of-life care.
Just last week, a grieving son asked me how it is even possible that the last two months of his 93-year old mother’s life could cost $200,000 in medical bills when his mother, suffering from fatal cancer, wanted no further extraordinary treatment. Surely there is a better way. But what are the solutions?
Cost of healthcare is a challenging issue because solutions often suggest fewer services or “less care.” But increasingly, we learn that is not the case; they can mean more appropriate care. Cost discussions become especially sensitive when it centers on care and treatment at the end of life. But in reality cost is an issue —– especially when tied to futile spending which detracts from the patient’s wishes and the dignity of death and dying.
Part of the cost problem is the low barrier to expensive, but truly miraculous and potentially life-saving, technology. I have lived it. My medical specialty included lung transplants, artificial hearts, and mechanical extracorporeal circulation. Such advances have tremendously improved American medicine. Over the last 50 years, average lifespan has increased two months every year! We live almost 10 years longer today than we did in 1960. We routinely transplant hearts into patients who would otherwise die within a month, and they live an additional 20 years. Fathers doomed to death live to watch their daughters marry and have children. But technology comes with a hefty cost, if misused.
Here are the facts: 30 percent of Medicare dollars are spent in the last months of life. That amounts to more than $150 billion annually. On top of that, a quarter of Medicare recipients spend more than the total value of all their assets on out-of-pocket health care expenses during the last five years of their lives. Every day in an intensive care unit can cost $10,000. Nearly 1 in 5 Americans spend their last days in an ICU.
Technology and intensive care treatment have limitations when misapplied. People spend fortunes on the last months of life. The high expectations and demands of grieving family members fuel this process. And because someone else is always paying, it is inevitable that unnecessary tests and procedures and high-intensity services creep into the equation. The system is set up and incentivized to bend to the whim of an unusual family member’s demand to “keep mom alive at all costs,” even if she is 93 and hopelessly ill.
So how do we fix all this? We begin a national, high-profile, civil dialogue, which should begin in the living rooms of patients and their families and extend to nurses’ and doctors’ offices, hospitals, religious institutions, and policy chambers. “How do I want to die?” That’s the framing question. It’s a tough place to start, but grounds the discussion in the reality that unless we act, our final days will be spent very differently than we would like.
Ventilators, mechanical heart assist devices, high-tech intensive care units, and powerful medicines provide the means of postponing the inevitable, usually uncomfortably and at high cost, while stripping away independence and dignity from those final days. Do we want to die at home or strapped to machines in a hospital bed? How much quality of life, how much loss of normal function, are we prepared to live with? Does my husband or daughter know my wishes?
Here are three proposals we should include in the conversation.
1.
Each of us must act to assume responsibility for expressing our preferences and intentions up front. Act today. Begin with establishing a written “advanced directive” to make your intentions clear. One type of advanced directive is a living will, which applies if you become incapacitated and lack competency to decide medical questions for yourself. Another important advance directive is the “durable healthcare power of attorney,” which designates a person to make medical decisions for you if you have not signed a living will or other directive.
Four out of five of us have not done this. These important legal documents provide an essential roadmap for your preferences and relieve your family and your doctors from having to guess what you would really have wanted and help resolves conflicts among family members. Share your values and intentions directly with your doctor, your family, and leader in your life.
2.
Medical education for our caregivers must be reformed to more specially address end-of-life issues. Many doctors and nurses are inadequately trained to lead families though these challenging times. How do you determine when further care is futile and then compassionately communicate the moment when technology adds no value, and in fact detracts from the dignity of life? How do you handle the well-intended-but-unreasonable family member who demands “more care” when the science says it’s futile? A physician, nurse, or hospital will worry about a lawsuit if the armamentarium of high technology is not exhausted even though evidence-based medicine says it is a waste of resources.
My physician dad and earlier generations of doctors were not confronted with a health service environment so complex and replete with alternatives as ours. In their day, medical science was inexpensive and limited in scope. They had less technology at their fingertips. Today’s physician requires more training in end-of-life communication and evidence-based decision-making.
3.
Expand both palliative and hospice care. Hospice provides compassionate and appropriately specialized care for those who will soon die. The setting is typically at home. Palliative care is a new specialty grounded on a multifaceted team-approach to comprehensively manage severe, often long-lasting chronic disease and persistent pain and suffering. Both center on autonomy and dignity and appropriate medical and social care for a particular patient’s medical condition. Both are based on science and evidence-based medicine. Both have been shown to improve patient satisfaction, reduce pain and discomfort, and improve quality of life.
Expansion will require rethinking reimbursement mechanisms to allow scalability. How do these two models fit within more integrated health systems? How should caregivers be compensated for providing more appropriate care but not more procedures and more technology?
Isaac Asimov wrote, “Life is pleasant. Death is peaceful. It is the transition that is troublesome.” It is time to focus on the transition. No one has the answers yet. But we can find them together. The way to begin is to initiate a rational national dialogue, as uncomfortable as the conversation may seem to be.
Dr. William H. Frist is a nationally acclaimed heart transplant surgeon, former U.S. Senate Majority Leader, the chairman of Hope Through Healing Hands and Tennessee SCORE, professor of surgery, and author of six books. Learn more about his work at BillFrist.com.
This article was originally featured in The Week http://theweek.com/article/index/233111/how-do-you-want-to-die
How the U.S. Can Find and Train More Great Teachers
(The Week, April 10, 2012)
By Bill Frist, M.D.
Consider Laura. When she entered the third grade, she couldn’t understand the stories all her friends enjoyed. She was even too embarrassed to read aloud. Why? She could only read at a first grade level.
Laura’s hardly alone — but that’s small comfort. A recent study from the Annie E. Casey Foundation found that one in six children who are not reading proficiently by the third grade does not graduate from high school on time. In other words, Laura’s abilities in third grade may very well determine her future.
By the time Laura finished third grade, however, she loved to read and was prepared for the fourth grade. How did she catch up? She had a highly effective teacher.
There are no silver bullets in the education reform movement, but one area we cannot afford to overlook is expanding the pool of talented teachers. Popular reform efforts tend to focus on supporting current teachers and improving the standards they teach. But to maximize Laura’s chances, and those of our country, we need to start even earlier.
Our lack of teacher accountability is akin to a drug company producing medicines without measuring if the pills actually cure disease.
Research shows that the No. 1 school-based factor in improving student achievement is a great teacher. Of course, other factors are important as well: High standards, strong school and district leadership, and parent and community involvement, to name a few. But great teaching is the lever that most dramatically changes the trajectory of a child’s future.
To foster great teaching, first we need to know what makes a great teacher. And the good news is, we’re making headway in better understanding teacher effectiveness. Many states are implementing new systems to evaluate teachers, designed to give them feedback on how they are doing and a clear picture of what they can improve on. These evaluation methods replace antiquated approaches in which teachers received feedback only once every few years — feedback that had little connection to what students were learning or to the day-to-day operations of a classroom.
But evaluations alone are of little use without providing the support for a teacher to improve. Thus, many of these new evaluation systems are being connected with professional learning to help teachers continuously improve, as is done in many other industries. Weaknesses identified through these new evaluations are addressed with ongoing, collaborative support, as teachers work in teams to improve their instruction.
Many school districts have also begun to reward teachers for effective teaching, paying them more if they are able to substantially improve student performance. Laura’s teacher, for instance, might see a bonus at the end of the year for the kind of dramatic achievement she brought forth in her students. This replaces the traditional and still-common system in which all teachers with similar education and years of service are paid the same, regardless of how effective they are at actually teaching. The concept of performance-based pay is not new, only new to teaching.
Identifying and rewarding great teaching is critical, but the reform movement is failing to tackle a third important area — focusing on the start of the teacher pipeline and growing the pool of better-prepared teachers before they enter the classroom. U.S. Secretary of Education Arne Duncan said last year that “unfortunately, we all know that the quality of teacher preparation programs is very uneven in the U.S. In fact, a staggering 62 percent of all new teachers — almost two-thirds — report they felt unprepared for the realities of their classroom.” Let’s better prepare our teachers before they enter the classroom by raising the quality of programs that train teachers to teach.
Here are three ways.
We must first enhance accountability in teacher preparation programs by tracking the success and effectiveness of candidates once they begin teaching. Most programs have no idea how their products, the teachers, actually fare in educating students over the ensuing years. This would be like a drug company producing medicines without measuring if the pills actually cure disease.
Second, we must align the curricula of teacher prep programs with the most current, innovative, and proven policies, so that teachers are prepared to teach effectively from the moment they first step into the classroom. There will always be on-the-job training, but our teachers should not have to start over from square one weeks after they themselves graduate.
Preparation should include the use of new teacher evaluation systems which highlight what effective teaching looks like, training on the use of data to improve classroom instruction, and robust preparation to teach the new Common Core State Standards, the state-led higher academic standards being implemented today in 45 states and the District of Columbia.
Third, it’s time to fully open the door to alternative teacher training programs, like Teach for America, that are able to recruit, train, and inspire effective teachers in a short period of time. More collaboration between alternative programs and traditional programs would allow for the sharing and replication of best practices across all teacher training programs.
Yes, all this takes time, and won’t be easy. But the time is ripe for systemic change to identify, prepare, support, and reward great teachers. Research suggests the results will be dramatic for kids. All must participate in this work — teachers and principals, backed up with a lot of backbone from policymakers. But remember: Catching up students like Laura and better preparing millions of other students for college and a career is worth the work.
Dr. William H. Frist is a nationally acclaimed heart transplant surgeon, former U.S. Senate Majority Leader, the chairman of Hope Through Healing Hands and Tennessee SCORE, professor of surgery, and author of six books.
This article was originally featured in The Week http://theweek.com/article/index/226586/how-the-us-can-find-and-train-more-great-teachers
SCORE Joins Highlands Town Hall Debate 2010
COOKEVILLE — The Highlands, Nashville’s WTVF NewsChannel5, Tennessee Tech University, and the League of Women Voters of Tennessee today announced that the State Collaborative on Reforming Education (SCORE) is joining as a sponsor in the Highlands Town Hall Debate 2010, a general-election gubernatorial debate scheduled for September 14 at TTU in Cookeville.
SCORE, a not-for-profit, non-partisan group led by former U.S. Senate Majority Leader Bill Frist, encourages sound education policy decisions at the state and local levels. Earlier this year, in January, the group co-sponsored a NewsChannel5 gubernatorial debate that included all major candidates in the Democratic and Republican primary fields.
“SCORE has a track record of promoting a non-partisan focus on important issues in this election,” Sandy Boonstra, news director of NewsChannel5, said. “We’re pleased to work with them once again.”
Frist, a surgeon who represented Tennessee in the U.S. Senate for 12 years, said SCORE supports a renewed focus on key issues, including education and health care. “Ensuring a better education for Tennessee students is critical as we work to improve health outcomes and promote a better quality of life for all Tennesseans,” he said. “SCORE is proud to support an open dialogue on the important issues in this election.”
As the first televised general-election gubernatorial debate held outside of Nashville, Memphis, or Knoxville, the Highlands Town Hall Debate 2010 will give focus to hometown issues facing rural and suburban areas — with an emphasis on economic development, education, and health care. The Highlands is a public/private economic development initiative between Overton, Putnam, and White Counties managed by the Cookeville-Putnam County Chamber of Commerce.
Using guidelines established by its partners, the debate will offer a unique perspective on voter attitudes by soliciting video questions in advance via YouTube and allowing Tennesseans to vote on which questions they want asked of the candidates. Written questions may also be submitted via the debate’s web site. The debate will include a section for live audience questions and a section for candidate-to-candidate questions.
On the Web: www.HighlandsDebate2010.com.
BlueCross BlueShield of Tennessee Pledges $500k to SCORE
BlueCross BlueShield of Tennessee today announced a $500,000 contribution to advance K-12 public education reform — and better health outcomes — in partnership with the State Collaborative on Reforming Education (SCORE), founded by former U.S. Senate Majority Leader Bill Frist.
“BlueCross BlueShield has a history of supporting promising community work across Tennessee, especially when it has the potential to promote better health,” said Vicky Gregg, president and CEO of the not-for-profit health plan. “Supporting a strong K-12 public education system is one of the best strategies for ensuring better health for the next generation.”
Gregg added: “BlueCross BlueShield is proud to partner with Sen. Frist and SCORE in their effort to support key education reform policies and promote school improvement on a statewide basis.”
SCORE is a nonprofit nonpartisan organization that works with state government and local school systems to encourage sound policy decisions in K-12 public education. Based at the John Seigenthaler Center at Vanderbilt University, SCORE provides policy and research support, and advocates on a statewide basis for key education reform initiatives including Tennessee’s First to the Top strategy.
Frist, one of 14 U.S. healthcare leaders serving on the Robert Wood Johnson Foundation’s Commission to Build a Healthier America, said a growing body of researchconfirms that people with more education are likely to live longer, experience better health outcomes and practice healthier behaviors.
“There is an undeniable connection between education and health,” said Frist, a surgeon who represented Tennessee in the U.S. Senate for 12 years. “That’s why now, more than ever, we need a public education system producing more high-school graduates who are better prepared for a career or college, and life.”
Frist added: “BlueCross BlueShield’s generous contribution to SCORE sends a powerful message about the strong link between improving educational attainment and ensuring better health outcomes.”
In addition to chairing SCORE, Frist serves as vice chair of the Partnership for a Healthier America, which leads First Lady Michelle Obama’s national campaign to fight childhood obesity. To support the national strategy, Frist and SCORE are exploring new public initiatives to promote healthy kids and healthy communities in Tennessee and the South.
“BlueCross BlueShield’s support is invaluable as we look to further strengthen the connection between education and health,” Frist said. “SCORE looks forward to working with the statewide healthcare community to ensure a smarter, healthier generation of Tennesseans in the years ahead.”
ABOUT BLUECROSS BLUESHIELD
BlueCross BlueShield of Tennessee is the state’s oldest and largest not-for-profit health plan, serving nearly 3 million Tennesseans. Founded in 1945, the Chattanooga-based company is focused on financing affordable health care coverage and providing peace of mind for all Tennesseans. BlueCross serves its members by delivering quality health care products, services and information. BlueCross BlueShield of Tennessee Inc. is an independent licensee of BlueCross BlueShield Association. For more information, visit the company’s Web site at www.bcbst.com.
ABOUT SCORE
The State Collaborative on Reforming Education (SCORE) serves as a resource for state government and local school systems. SCORE is committed to thoughtful advocacy and policy work, and to building and sustaining a diverse coalition of public- and private-sector partners. SCORE is governed by a 14-member board of directors, chaired by Sen. Frist and comprised of Tennessee philanthropic and business leaders who care about public education.
Frist’s Statement on Race To The Top.
NASHVILLE – Former U.S. Senate Majority Leader Bill Frist, who chairs the education-reform group Tennessee SCORE, on March 4 issued this statement following news that Tennessee is a finalist in the federal government’s groundbreaking Race to the Top competition:
“Tennessee’s spot as a finalist confirms what we’ve known: The Volunteer State is poised to move farther, faster in public education reform than any other state in the nation. Governor Bredesen, the General Assembly, and stakeholders including the TEA are to be commended for their bipartisan work in positioning us for success. Thanks also to Secretary Duncan and the U.S. Department of Education for recognizing the extraordinary opportunities that exist here. Statewide, the education-reform community stands ready to help make sure that Tennessee is ‘first to the top.”
The Tennessee State Collaborative on Reforming Education (SCORE) is a nonprofit, nonpartisan organization that promotes education innovation. In October 2009, SCORE released “A Roadmap to Success,” a report outlining comprehensive strategies for improving Tennessee schools. Many of the strategies were adopted in January’s special legislative session on education reform.
SCORE Final Report
On October 22, 2009, SCORE released its Final Report entitled ‘A Roadmap to Success: A Plan to Make Tennessee Schools #1 in the Southeast Within Five Years.” The report lays out in detail a plan that includes four key strategies that will help Tennessee become the Southeast’s top education performer – embracing high standards, cultivating strong leaders, ensuring excellent teachers, and utilizing data to improve student learning. It also outlines the role various groups can play in improving our schools. To download a copy of the report, please click here.
Tennessee Race to the Top Application Summary
SCORE has written a six-page summary of Tennessee’s 1,111-page Race to the Top application. This summary does not reflect SCORE’s view on the individual components of the application but rather is an attempt to summarize the application in a concise way. To view the summary, please click here. To view the complete application, pleaseclick here.
SCORE Gubernatorial Forum on Education
On Thursday, January 14, 2010, the Tennessee State Collaborative on Reforming Education (SCORE), along with Nashville’s News Channel Five and Belmont University hosted the first major gubernatorial forum of the 2010 election year. The Gubernatorial Forum on Education was the first time all the main candidates for governor from both the Democratic and Republican parties gathered on the same stage, sharing their ideas and plans for education and economic development in Tennessee.
To view the forum online, please click here.
About SCORE
The Tennessee State Collaborative on Reforming Education (SCORE) is an initiative to jumpstart long-term educational change in Tennessee to ensure that every child graduates high school prepared for college or a career. SCORE is chaired by William H. Frist, former Majority Leader of the U.S. Senate, along with a 30-person Steering Committee. To read more about SCORE, please click here.
Frist Statement on Race to the Top
NASHVILLE — Former U.S. Senate Majority Leader Bill Frist, who chairs the education-reform group Tennessee SCORE, today issued this statement following news that Tennessee is a finalist in the federal government’s groundbreaking Race to the Top competition:
“Tennessee’s spot as a finalist confirms what we’ve known: The Volunteer State is poised to move farther, faster in public education reform than any other state in the nation. Governor Bredesen, the General Assembly, and stakeholders including the TEA are to be commended for their bipartisan work in positioning us for success. Thanks also to Secretary Duncan and the U.S. Department of Education for recognizing the extraordinary opportunities that exist here. Statewide, the education-reform community stands ready to help make sure that Tennessee is ‘first to the top.’”
The Tennessee State Collaborative on Reforming Education (SCORE) is a nonprofit, nonpartisan organization that promotes education innovation. In October 2009, SCORE released “A Roadmap to Success,” a report outlining comprehensive strategies for improving Tennessee schools. Many of the strategies were adopted in January’s special legislative session on education reform.
Special Session Presents Once-in-a-Lifetime Opportunity
By: Sen. Bill Frist, M.D.
In my 12 years of service to Tennesseans in the United States Senate, I learned that progress often comes from taking advantage of moments when the stars align around a specific goal. In Tennessee, one of those moments is upon us, as for the first time in over 25 years the stars have aligned to make real, meaningful improvements to Tennessee’s education system.
Today, there are a number of factors coming together to create a truly unique opportunity for improving our schools. Earlier this year, Governor Bredesen’s Tennessee Diploma Project went into effect, for the first time raising Tennessee’s academic standards to a nationally competitive level. At the same time, national foundations, who for far too long have ignored Tennessee, have started to make major investments in our schools. In the last six months alone, the Bill & Melinda Gates Foundation has committed $90 million to improving teacher effectiveness in Memphis and made several other smaller investments across the state.
Perhaps most importantly is the consensus that has been built over the past year about how to improve Tennessee’s education system. For the past year, I have chaired the Tennessee State Collaborative on Reforming Education (SCORE). Led by a 25-member steering committee of top education, political, and business leaders from across Tennessee, SCORE has gathered input from all the state’s key education stakeholders by holding 72 town hall meetings across the state, hosting eight statewide meetings with leading education reformers from around the country, and conducting hundreds of one-on-one interviews.
In late October, SCORE released a final report entitled “A Roadmap to Success: A Plan to Make Tennessee Schools #1 in the Southeast Within Five Years.” This report laid out the specific things each group – whether it be legislators, teachers, parents, or the business community – needs to do to improve our schools. Over 300 individuals offered feedback on this final report, which represents a bold consensus among the state’s education stakeholders about a detailed plan for improving Tennessee’s education system. Never before has there been so many different groups come together and agree about the way forward.
As members of the Tennessee General Assembly meet today in a special legislative session focused on education, I encourage them to take advantage of this truly unique moment in our state’s history. Now is the time to enact truly meaningful education reform. While the timing of the special session is in part driven by a desire to make the state’s application for federal Race to the Top funds more competitive, many of the ideas proposed in the current legislative package represent ideas that have been developed over the past year through SCORE’s inclusive process and wide-ranging outreach.
Specifically, SCORE’s final report laid out seven policy recommendations for the state legislature. These seven items make up a large portion of the proposals being recommended by Governor Bredesen and being considered in the General Assembly. Passing these items will not only ensure that Tennessee is competitive for hundreds of millions of federal Race to the Top dollars, but it will also ensure that Tennessee undertakes much needed education reforms that have been identified as necessary by many of Tennessee’s teachers, principals, superintendents, and maybe even more importantly, by parents and grandparents. From the classroom to the boardroom, everyone has an interest in seeing our schools improve.
The stars have clearly aligned in Tennessee to create a once-in-a-lifetime opportunity to improve our schools. My hope is that this legislative special session will bring everyone together to take advantage of this truly unique moment. If we all rise to the occasion, I am confident our schools will significantly improve and the children in our state will have a brighter future.
Bill Frist served as U.S. Senate Majority Leader from 2003- 2007 and is Chairman of Tennessee SCORE.
Bill Frist Receives 2011 NBAA Humanitarian Award
Bill Frist Receives 2011 NBAA Humanitarian Award from Bill Frist on Vimeo.
Bill Frist Flies Missions Worldwide to Help Those in Need
Esteemed doctor, pilot and former U.S. Senate Majority Leader Bill Frist has been awarded the National Business Aviation Association’s (NBAA’s) 2011 Al Ueltschi Award for Humanitarian Leadership in recognition of his life-saving efforts worldwide, and the importance of business aviation to those endeavors.
An accomplished medical researcher and heart transplant surgeon, Dr. Frist was elected to the Senate representing Tennessee in 1994, the first practicing physician elected to the lawmaking body since 1928. During his two terms in office, Frist rose to the majority leader position faster than any previous senator while spearheading efforts to improve medical access for Americans and others worldwide, notably leading on bills like the Medicare Modernization Act and the passage of the President’s Emergency Plan for AIDS Relief (PEPFAR). PEPFAR combats the spread of disease in resource-limited areas worldwide, and since its passage has provided life-saving anti-retroviral drug treatments to over 3.2 million people and counseling, testing and education to over 33 million to help prevent new infections. This ambitious program is often credited with saving a generation of Africans.
A true citizen-legislator, Frist has continued his regular medical mission trips worldwide since his retirement from the Senate in 2007. Frist – a pilot since the age of 16 and holder of multi-engine, commercial and instrument ratings – has consistently relied on aviation and his own piloting skills to expand his life-long commitment to healing to areas around the globe.
From using aviation night after night to personally transport hearts during his time-sensitive transplant procedures, to piloting planes throughout war-torn Sudan to perform surgery, Frist credits aviation as a powerful instrument for healing. Within days of the levees breaking in New Orleans after Hurricane Katrina, he flew his plane to care for those stranded. In flooded Bangladesh, he relied on floatplanes to ferry needed personnel and supplies on behalf of Save the Children and Samaritan’s Purse, and in 2010, he immediately flew to Haiti to perform surgery in the aftermath of the earthquake in Haiti.
“Bill Frist has combined his skill as an aviator with his expertise in medicine to reach people in need of life-saving treatment at home and all over the world,” said NBAA President and CEO Ed Bolen. “From piloting his own aircraft throughout Sudan to give surgical care, to using aviation to reach and treat victims days after the devastating earthquake in Haiti, the senator and doctor truly ‘walks the walk’ in assisting those most in need of help. He exemplifies the humanitarian spirit that’s always been a part of business aviation, and we are honored to recognize his pioneering work with this award.”
In his 2009 book Heart to Serve: The Passion to Bring Health, Hope, and Healing, Frist wrote about his belief that medicine unites the world in its common goal for peace. “People don’t usually go to war against someone who helped save their children,” he wrote. “While the world often sees America’s tougher side…when people see America’s more compassionate, humanitarian side, the barriers come down, and peace becomes a viable possibility.”
Established in 2006, NBAA’s Al Ueltschi Award for Humanitarian Leadership recognizes the spirit of service demonstrated by humanitarian leaders within the business aviation community. The award is named for Albert L. Ueltschi, who was instrumental in the development of ORBIS, an international non-profit organization dedicated to preventing blindness and saving sight.
The award will be presented to Frist at the Opening General Session for NBAA’s 64th Annual Meeting & Convention (NBAA2011) in Las Vegas, scheduled for 8:30 a.m. on Monday, October 10, 2011. The full Convention will be held Monday, October 10 through Wednesday, October 12.
Past recipients of the Al Ueltschi Award for Humanitarian Leadership include Cessna Aircraft Company (2006), the Veterans Airlift Command (2007), Corporate Angel Network (2008), and the Civil Air Patrol (2009). Last year, the Association honored humanitarians throughout the business aviation community for their efforts in providing relief efforts following the earthquake that devastated Haiti in January 2010.
# # #
Founded in 1947 and based in Washington, DC, the National Business Aviation Association (NBAA) is the leading organization for companies that rely on general aviation aircraft to help make their businesses more efficient, productive and successful. The Association represents more than 8,000 companies and provides more than 100 products and services to the business aviation community, including the NBAA Annual Meeting & Convention, the world’s largest civil aviation trade show. Learn more about NBAA at www.nbaa.org.
Members of the media may receive NBAA Press Releases immediately via e-mail. To subscribe to the NBAA Press Release e-mail list, submit the online form atwww.nbaa.org/news/pr/subscribe.
In Case You Missed It… RealClearPolitics : Newsmaker Interview with Bill Frist
RCP: Republican candidates are pledging to repeal the health care bill, and with your background in medicine and also as a leader in the Senate acutely aware of policy-making, what’s the best way for Republicans to proceed?
Frist: Republicans will not repeal the fundamentals of the new law. Because of the law’s unpopularity with so many hard-working, centrist voters, who see their health cost and taxes continuing to rise, the mantra of “repeal and replace” resonates at election time. Republicans will pick up 500 state legislative seats, the majority of governorships, and will regain control of the House. In two weeks, they then become the leaders of the legislative branch. The electorate wants results and their responsibility will be to constructively shape implementation of the new law.
RCP: If they try to repeal parts of the bill, what parts will they start with, and what is realistic?
Frist: Passing a law is 20% of the work (the easy part). Implementing it successfully requires 80% of the effort. As with Medicare and Medicaid in the 1960’s and 1970’s, implementation will ultimately be defined by regulatory language, interpretation of Congressional intent, and the outcome of elections (in this case, a series of elections in 2010, 2012, 2014, and 2016).
Repeal of discrete sections of the law are a possibility but will require solid bi-partisan support. For example, consideration will be given to repeal (or modification of) the Independent Payment Advisory Board. Is it too much power to allow 15 unelected individuals the absolute authority to unilaterally dictate with the force of law how to cut Medicare for as much as 2% a year every year?
RCP: What parts of this bill are solid and should stay in place if changes begin?
Frist: The “individual mandate,” the redefinition of the Medicaid coverage threshold to be 133% of poverty, the demonstration projects of accountable care organizations and medical homes, payment reform, and prevention are solid.
RCP: Do you think Republicans have been entirely correct in how they’ve portrayed the bill; do you think there misperceptions remain about the law as Democrats suggest?
Frist: Those who call the law a federal government takeover are wrong. Yes, there are more government mandates, bureaucracies, and hefty government spending, but our health care sector will maintain its rugged pluralism and its strong employer-based foundation (150 billion people). Care will continue to be delivered by non-government physicians and nurses working in non-government hospitals and facilities.
RCP: What new legislation would you like to see crop up regarding health care delivery in this country?
Frist: The health sector needs breathing room from new legislation. For innovation to prosper, new cost-effective treatments to emerge, accountable care organizations to be established, state exchanges to be operationalized, more laws are not needed. The sector needs some certainty and time to adapt.
RCP: How big of a role do you think health care and the new law will factor into the Republican presidential primary over the next year, and how do you think it will shake up the field?
Frist: The next presidential election will be determined by 2 things: the economy/jobs and Afghanistan. Health care will not be a defining issue in the presidential election in 2 years, but will be cited by voters as supporting evidence of one’s own views on taxes, the role of government, and entitlement spending (the debt).
RCP: If a Republican unseats President Obama in 2012, what’s the first step that president should take regarding health care policy?
Frist: The President must focus “like a laser beam” on health care costs. This will likely begin with provider payment reform which will transform fee-for-service, volume-based payments to value-based constructs. Incentives and markets will work. Government fiat will not.
RCP: What is being ignored currently in the implementation of the health care bill/what do you think will crop up in the debate in the next few years that we’re missing now?
Frist: The law is state-driven, not federally driven. Both the 16 million new entrants to Medicaid and the 24 million in the new health exchanges will be state-administered. Today, the federal government is inadequately serving the states in view of the huge (and I’d argue appropriate) responsibility it has thrust on the states.
RCP: What is the best way to curb health care costs in your view?
Frist: Markets and incentives. When fairly framed by government, they work. Just look at the Medicare Modernization Act of 2003. With transparency, competition, incentives, partnership with the private sector, prescription drug costs for seniors with Medicare have year after year have come in 10 – 20% less than predicted. That is bending the cost curve.
RCP: You’re still very involved in health care policy in the country from Tennessee; what’s topping your agenda on health care policy and what you will be doing over the next few years?
Frist: My life is health. I spend a third of my time on health care policy, a third on global health issues like children’s issues and clean water through Hope Through Healing Hands, and a third marrying private capital to dynamic managers who are constructively and innovatively addressing the “value equation” in health care. I loved transplanting hearts and I love transforming health care.
To read the entire interview on RealClearPolitics, please click here